Discover our programs:
For Members of participating funds with a body mass index (BMI) ≥ 28 who have knee or hip osteoarthritis or joint pain requiring surgery.
For Members of participating funds with a body mass index (BMI) ≥ 28 who have a cardiovascular condition (includes high blood pressure, high cholesterol, irregular heart beat and blockages).
For Members of participating funds with a body mass index (BMI) ≥ 28 who have type 2 diabetes.
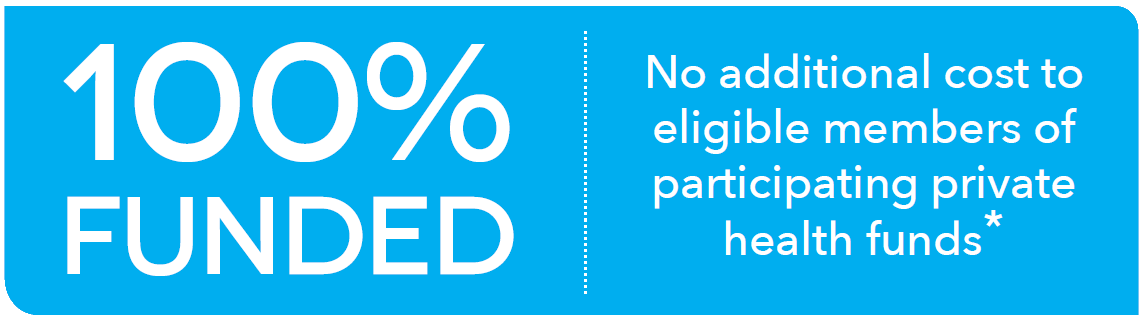
* Clinical and policy eligibility criteria apply. Waiting periods apply.
Member stories
Robyn at week 18
The program offers great support and delivers on its promises. I think it is wonderful that HCF have provided me with the opportunity to do this program. The trajectory I was on in my mid 50’s was not a healthy one, which would have led to health issues later in life. It works! It is educational, provides excellent support and is packaged and presented in a way that there are no excuses. The team members I have contacted have been wonderful - positive and informative - providing strategies to keep me on track.
Shirley at week 18
It is an easy to follow and well supported program. The information and guidelines provided are realistic, providing everyday support and explanations. The way the breakfast, lunch and dinner options were listed was so easy to follow and remember for future reference. The book is a great asset to the program with very revealing information for use in life. It is easy to apply and doesn’t require anything special. A wonderful educational program!
Janet at week 18
I am so grateful for the OAHWFL program. I lost 10kg and 9 inches around my waist in the 18 weeks, thanks to the meal replacements and recipes and dietary advice. I had tons of energy and got motivated to exercise more. My hip replacement was last Feb, and I now ride 4kms on the cycle path every second day or so, and enjoy it. I lost a whole clothing size and feel healthy. Best of all, my hip pain is negligible and my chronic back pain is much less frequent. I can perform pretty much all household and gardening tasks that I was doing 2-3 years ago before my hip got bad.
Denis at week 18
It helped me drop blood pressure medications, more energy and overall well being. Fitter than I was 18 weeks ago, dropped 10cm off belt size!
Meredith at week 18
Thank you for the opportunity to participate in the Osteoarthritis Healthy Weight For Life program.
It has been life changing for both of us. I look in our pantry and the change is amazing. No more sweet biscuits, no snacks, no treats. More cans of beans etc for salads. Sugar is lasting twice as long as before and without a doubt the best tool has been the plate divider.
Frank is so much more mobile and has regained a confidence I have not seen for a very long time. He has increased his exercises (group based) and moves virtually independently within the house.
Other health issues have decreased dramatically and I can pinpoint the program as being the catalyst for improvement.
We are both grateful to have been offered this program and are determined to maintain the improvements we have achieved. We are both healthier, happier and a lot more mobile than in July/ Aug when we started.
Glen at week 18
This program has been very effective in assisting me to NOT require Total Knee Replacement (TKR) surgery. This is a major factor in my improved sense of well-being achieved throughout the last 16 weeks. I was scheduled by one orthopaedic specialist to undergo TKR on the 25th October, and, after seeking a 2nd opinion, that specialist clearly adopted a different paradigm to rushing to surgery. This has been so important, and my knee pain has improved significantly, as evidenced in my return to 'normal' activities' and reflected in my survey responses over time. My GP has been extremely impressed, and, most importantly, the impact of the support has been critically important in my not requiring TKR surgery, which has substantial risks and potential complications.
Dragana at week 18
"It helped me to lose ~17 kilos, my glucose levels are in normal ranges, my cholesterol reading much better and I feel full of energy almost all the time. I couldn't be happier with the results."
Tom at week 18
I have lost around 24KG so far, this is the most effective diet I have ever been on, my BSL is now around 6.4 from 13-16 and I am off insulin and have reduced my Metformin and BP meds as BP has now improved and are now also off Rabeprazol which I had to take for acid reflux which I no longer have.